What Medicare Is and How to Get It: A Breakdown
What Is Medicare?
Medicare is a federally facilitated health insurance program for people age 65 and older and younger persons with disabilities or end-stage renal disease (ESRD). Medicare was first enacted in 1965 by President Lyndon B. Johnson and included Medicare Part A and Part B insurance, known as Original Medicare.
Medicare Parts A and B cover many of your healthcare services and devices, but they don’t pay for everything. For instance, Parts A and B don’t cover services like dental work, routine eye exams and out-of-pocket costs, such as deductibles, coinsurance, and copayments.
Medicare Has Changed Over Time
 Understanding Medicare also involves learning about changes that have expanded Medicare eligibility and coverage. The first major change came in 1972 when President Nixon signed an expansion into law that allowed for the inclusion of those with disabilities and ESRD.
Understanding Medicare also involves learning about changes that have expanded Medicare eligibility and coverage. The first major change came in 1972 when President Nixon signed an expansion into law that allowed for the inclusion of those with disabilities and ESRD.
The 1980s marked the enlargement of home health services, which included the addition of hospice benefits for the terminally ill in 1982. The 80s was also the time period when Medicare Supplement plans were standardized by the federal government.
During the 1990s, new legislation made it possible for Medicare-eligible people to get Medicare through private plans that included extra benefits, such as prescription drugs. These plans were called “Medicare+Choice,” and later became known as Medicare Advantage.
In the early 2000s, individuals under age 65 diagnosed with amyotrophic lateral sclerosis (ALS), also called Lou Gehrig’s disease, became eligible for Medicare, and the Medicare Prescription Drug Improvement and Modernization Act of 2003 was signed into law by President George W. Bush. Later on, the Patient Protection and Affordable Care Act of 2010 made several reforms in an effort to increase services, manage costs, and improve delivery of the Medicare program. The reforms also added free preventive benefits to Medicare and improved prescription drug coverage.
What Medicare Is Not
Medicare is not a “free” health insurance program. Although you can get extra help with paying for Medicare premiums through certain assistance programs, you still have other out-of-pocket costs. A type of government-run health insurance program that can be free or provided at a low cost for certain people is Medicaid. You can qualify for Medicaid based on your family size and whether you meet certain low-income requirements. And, unlike Medicare, which is mostly for people age 65 and older, Medicaid is for people of all ages (including children). The infographic below shows more differences between Original Medicare and Medicaid.
Understanding Medicare Parts
Answering the question, “What is Medicare?” requires understanding the four Medicare parts: A, B, C, and D. Each part provides different benefits, has specific enrollment requirements, and has different costs. Let’s look at a summary of the different Medicare parts.
- Part A: Hospital insurance administered through the Medicare program
- Part B: Medical insurance administered through the Medicare program
- Part C: Hospital and medical insurance, plus potential additional health benefits administered through private insurance companies
- Part D: Prescription drug coverage administered through private insurance companies
What Is Medicare Part A?
Medicare Part A is insurance that covers inpatient hospital care, inpatient stays in most skilled nursing facilities, hospice care, and home health services. Medicare Part A coverage is funded through payroll taxes such as the Federal Insurance Contributions Act (FICA) tax—approximately 1.45 percent of your earnings get paid into FICA. It’s also funded through other means, including income taxes you pay on Social Security benefits.
What Does Medicare Part A Cost?
Medicare Part A coverage doesn’t have a monthly premium if you or your spouse worked in the U.S. and paid taxes to Medicare for at least 10 years. If you do have to pay a premium, it can cost you up to $548 a month. But the premium can be up to 10 percent more than the usual amount if you don’t qualify for premium-free coverage and you didn’t enroll in benefits when you first became eligible. In addition to the monthly premium, you pay an annual deductible of $1,408 for each benefit period.
What Is Medicare Part B?
Medicare Part B is health insurance for Medicare enrollees that covers medically necessary and preventive care. This includes things like doctor visits, partial hospitalization mental health care, ambulance services, durable medical equipment, breast cancer and colorectal cancer screenings, glaucoma tests, and limited outpatient prescription medicines.
Funding for Part B Medicare comes from a budget authorized by Congress, including premiums you pay for Part B and Part D coverage. A difference between Medicare Part A and B is that you must pay a monthly premium to maintain Part B coverage.
What Does Medicare Part B Cost?
The standard premium for 2020 is $144.60, but it can cost more based on your income and tax filing status. You also pay an annual Part B deductible of $185, and a 20 percent coinsurance for covered medical services after you’ve met your deductible. The chart below shows the premium rate for Part B based on 2016 annual earnings.
| 2020 Part B Monthly Premium | 2018 Annual Income | ||
|---|---|---|---|
| If Filed Individual Tax Return | If Filed Joint Tax Return | If Married and Filed Separate Tax Returns | |
| $144.60 | $87,000 or less | $174,000 or less | Less than $87,000 |
| $202.40 | $87,001 – $109,000 | $174,001 – $218,000 | N/A |
| $289.20 | $109,001 – 136,000 | $218,001 – $272,000 | N/A |
| $376.00 | $136,001 – $163,000 | $272,001 – $326,000 | N/A |
| $462.70 | $163,001 – $500,000 | $326,000 – $750,000 | $87,001 – $413,000 |
| $491.60 | More than $500,000 | More than $428,000 | More than $413,000 |
Medicare Part A and Part B Eligibility and Enrollment
 Parts A and B are available to you when you turn 65, or when you’ve been receiving Social Security Disability benefits for at least two years. You’re usually automatically enrolled in both parts if:
Parts A and B are available to you when you turn 65, or when you’ve been receiving Social Security Disability benefits for at least two years. You’re usually automatically enrolled in both parts if:
- You’re already getting benefits from Social Security or the Railroad Retirement Board (RRB)
- You have amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease
- You’re under 65 and receiving disability benefits
- You’re a resident of Puerto Rico who gets Social Security or RRB benefits
You’ll know that you’ve been automatically enrolled if you get your Medicare card in the mail three months before you turn 65 or during your 25th month of disability.
If you’re not automatically enrolled, you can sign up during your Initial Enrollment Period (IEP). Your IEP lasts 7 months and is made up of the three months before and after your 65th birthday and your birthday month. You can also sign up for Medicare Part A and Part B during the General Enrollment Period (GEP), which runs from January 1 to March 31 each year. Another difference between Medicare Part A and B is that if you don’t sign up for Part B during your IEP, you will most likely pay a late enrollment penalty for the entire time you have Part B coverage.
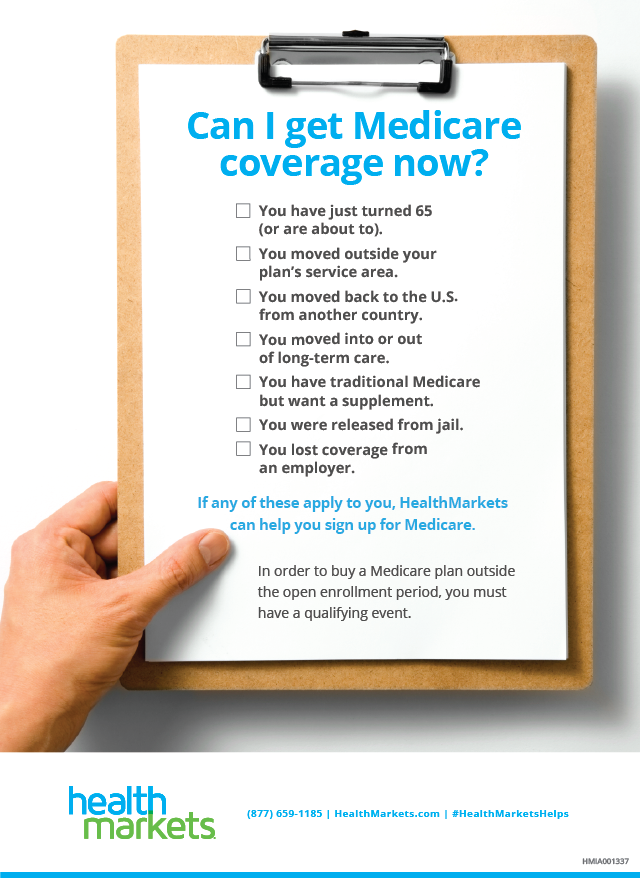
Medicare Special Enrollment Periods
Outside of the IEP and GEP, you can also enroll in Medicare Parts A and B (as well as the other Medicare parts) during Special Enrollment Periods (SEPS) if you experience a qualifying life event. There are several types of life events that qualify as SEPs for Original Medicare, Medicare Part C, and Medicare Part D. Some examples are below.
What Is Medicare Part C?
The first thing to know about Medicare Part C (also called Medicare Advantage) is that it includes both Medicare Part A and Part B benefits (except hospice care, but Original Medicare covers that for people with Medicare Advantage). Plans can also include additional benefits, such as nursing home and assisted living facility care, prescription drugs, vision, hearing, and dental coverage. In most cases, Medicare Advantage plans have networks of doctors and hospitals, much like employer-provided insurance plans.
Enrolling in Medicare Part C
You must have Medicare Parts A and B to be eligible for Part C. Typically, you can’t enroll if you have ESRD. Like Parts A and B, you can sign up for Medicare Part C during your IEP when you turn 65 or are under 65 and have a disability. If you enrolled in Part A during your IEP and sign up for Medicare Part B for the first time during the January 1 to March 31 GEP, you will become eligible for Medicare Advantage during the Part C and Part D GEP, which runs from April 1 to June 30. You can also get Medicare Part C coverage by switching from Original Medicare to Medicare Advantage during the Medicare Annual Election Period (AEP), also called Medicare Annual Enrollment Period or Medicare Open Enrollment Period.
Medicare Part C Plan Options
Because Medicare Advantage plans are sold by private insurance companies, the types of plans available vary from company to company. Options generally include a choice of an HMO, PPO, HMO-POS, PFFS, SNP, or Medicare MSA plan. Let’s break each down.
HMO—A Health Maintenance Organization plan requires having a primary care physician (PCP) and getting a referral from the PCP to see a specialist. Services are usually limited to doctors within the plan’s network, which helps to lower the cost.
PPO—Preferred Provider Organization plans don’t require a referral to see a specialist. Coverage is available at both in- and out-of-network providers, but you usually pay a higher portion of the costs for going out-of-network. Monthly premiums are usually higher than that of an HMO.
HMOPOS—This plan combines traditional HMO coverage with Point of Service benefits by allowing you to go outside the plan’s network for certain services in exchange for a higher out-of-pocket cost.
PFFS—Private Fee-For-Service plans can also have in-network and out-of-network providers. These plans don’t require you to select a PCP or get a referral to visit a specialist. With PFFS coverage, the plan decides how much it will pay providers and what your share of the costs will be for covered services.
SNP—Special Needs Plans are often available only to those with limited incomes or specialized health needs and have benefits tailored to meet those needs.
Medicare MSA—A Medicare Medical Savings Account combines a high-deductible Medicare Part C plan along with an account you can use to help pay out-of-pocket healthcare costs. This type of plan requires that you pay an annual deductible before the plan starts to pay for covered services.
What Does Medicare Part C Cost?
Medicare Advantage premiums depend on where you live and the type of plan you have. Typically, plans that have more restrictions (such as an HMO) will cost less, while plans that have more flexibility (such as a PPO) will cost more. In 2019, for example, the monthly premium weighted by enrollment was $23 for an HMO plan and $39 for a local PPO plan.
Medicare Advantage plans can have a $0 monthly premium. Medicare Advantage plans can have a $0 premium if an insurance company saves money on healthcare costs from contracts it has with providers and decides to pass on those savings to plan members. In learning about Medicare Part C $0 premiums, it’s important to understand that having a $0 premium doesn’t mean the plan is free. You still have to pay out-of-pocket costs, such as your copayments and coinsurance. Plus, you continue to pay your Part B Medicare premium when you’re enrolled in Medicare Part C coverage.
What Is Medicare Part D?
Medicare Part D is outpatient prescription drug coverage for Medicare beneficiaries. Signing up for Part D coverage is voluntary. However, because most prescription drugs aren’t covered under Original Medicare, enrolling in Part D offers seniors and younger individuals on Medicare an affordable way to pay for prescription medicines. Every Part D prescription drug plan has a formulary of covered drugs, which can be brand -name or generic. But each drug formulary is unique, so some may only cover a specific type of brand- name or generic drug.
 How to Get Medicare Part D
How to Get Medicare Part D
You can only get Part D coverage through plans sold by private insurance companies. You can buy either a stand-alone Medicare Part D prescription drug plan (also called PDP) to add drug benefits to Original Medicare or buy a Medicare Advantage plan where Medicare Parts A, B, and D are combined. Advantage plans that include prescription drug coverage, which are the majority of plans, are known as Medicare Advantage Prescription Drug Plans (MA-PDs).
Eligibility and Enrollment for Medicare Part D
If you have Medicare Part A or Part B, you can enroll in a stand-alone PDP, an MA-PD or another Medicare Part D plan that provides prescription drug benefits during your IEP. You may pay a late enrollment penalty if you don’t enroll in a Part D plan or have other creditable drug coverage within 63 days of your IEP, unless you get extra help from Medicare to pay your drug costs.
If you didn’t enroll during your IEP, you have another chance to sign up for Part D benefits during the Medicare Open Enrollment Period. If you already have a Part D plan, this period is also the time when you can switch to a different one or drop your plan. Another important part of understanding Medicare Part D is that if you enroll in a Medicare Advantage plan that includes drug coverage (MA-PD) and then later enroll in a stand-alone prescription drug plan (PDP), you will be dis-enrolled from your MA-PD plan and re-enrolled back in Original Medicare.
What Does Medicare Part D Cost?
 The average monthly premium for a standalone Medicare Part D plan in 2019 was $33.19. Some drug plans also have a deductible that you must pay before the plan starts to cover your prescriptions. Once you’ve met the plan’s deductible (if it has one), the plan covers most of your prescription drug costs, and you pay a copayment or coinsurance until the total amount spent by you and your plan on covered drugs reaches a certain amount, which is $4,020 in 2020.
The average monthly premium for a standalone Medicare Part D plan in 2019 was $33.19. Some drug plans also have a deductible that you must pay before the plan starts to cover your prescriptions. Once you’ve met the plan’s deductible (if it has one), the plan covers most of your prescription drug costs, and you pay a copayment or coinsurance until the total amount spent by you and your plan on covered drugs reaches a certain amount, which is $4,020 in 2020.
What Is Medicare Part D Donut Hole?
When you reach the amount that you and your plan must spend on prescription drugs during a calendar year, you’ve entered the Part D coverage gap, known as the “donut hole.” While you’re in the Medicare Part D donut hole, you pay no more than 25 percent (in 2020) of the cost for covered brand-name drugs and covered generic drugs. However, not every Part D plan member will enter the donut hole, and those who receive extra help won’t enter it.
Getting Out of the Medicare Part D Donut Hole
You’re out of the coverage gap or donut hole when you’ve spent the maximum out-of-pocket amount for your prescriptions, which is $6,350 in 2020. Your stand-alone Medicare Part D prescription drug plan or MA-PD plan will automatically provide you with catastrophic drug coverage once you’re out of the donut hole. Catastrophic coverage covers most of the costs for high-priced medicines, or at least a much smaller cost for the remainder of the year.
What Is Medicare Supplement Insurance?
Medicare Supplement insurance, also called Medigap insurance, helps pay for expenses that Original Medicare doesn’t cover, which are mostly copays, coinsurance, and deductibles. Some plans also cover certain medical treatments you may get while traveling outside the U.S. There are 10 standardized Medigap plans categorized by letters: Plan A, Plan B, Plan C (which is only available to those were eligible for Medicare before January 1, 2020), Plan D, Plan F (which is only available to those were eligible for Medicare before January 1, 2020), Plan G (including a high-deductible option in some states), Plan K, Plan L, Plan M, and Plan N. With the exception of 3 states (Massachusetts, Minnesota, and Wisconsin) where Medigap plans are standardized differently, plan benefits are the same from state to state.
The chart below shows a comparison of the different Medigap insurance plans.

Your Medigap plan benefits kick in once Medicare has paid the approved amount for a covered service. Although Medigap plans can help supplement Original Medicare, they don’t cover costs for certain services and devices, such as long-term care, routine eye and dental care, private-duty nursing, eyeglasses, and hearing aids. To get these benefits, you can enroll in Medicare Part C coverage instead or buy a senior supplemental health insurance plan.
Medigap Insurance Eligibility and Enrollment
You’re eligible for Medigap insurance if you have both Medicare Parts A and B. The ideal time to enroll is during the Medigap open enrollment period, which starts in the month you turn 65 and are enrolled in Part B. This is because you can get any plan available in your state regardless of your health. But if you wait until this period is over, you have to go through medical underwriting to determine whether you can enroll in a plan.
Buying a Medicare Supplement Plan
Like Medicare Part C and Part D, Medicare Supplement insurance plans are sold through private insurance companies. Companies that offer any Medigap insurance must offer Plan A. In addition, the cost of Medicare Supplement insurance plans can be different based on the company as well as your geographic location.
Now that you have some answers to the question, “What is Medicare?,” you may be ready to take the next step by enrolling in a plan. Get started shopping online now to find a plan that is write for you, whether it’s a Medicare Advantage plan, a Medicare Part D prescription drug plan, or a Medigap insurance plan. This service is at no cost to you with no obligation to enroll.